Regular readers of this blog and followers on social media know that I was diagnosed with an intestinal infection due to clostridium difficile (commonly known as “c. diff“) about four months ago. In my last post, I shared the treatment up to that point and that the next step would be to undergo a fecal microbiotia transplant (FMT) and promised to write an update after that experience. It gives me great pleasure now to do that and to announce that I have now tested NEGATIVE for c diff and am definitely on the path to recovery.
First, let’s review…
What is clostridium difficile and how does it cause problems?
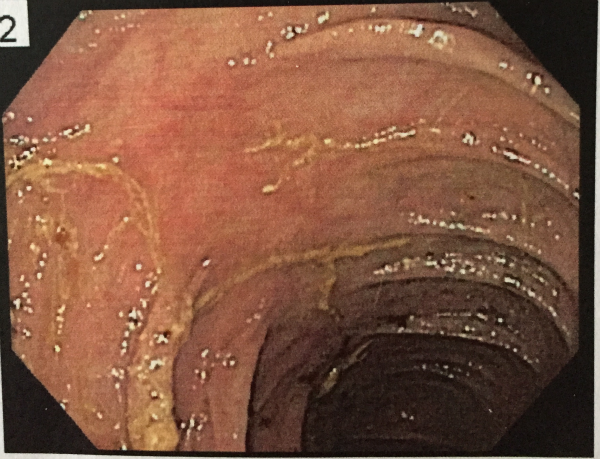
Clostridium difficile is a bacterium found in the intestines. It is believed that healthy people can and often do have the bacteria in their guts, but that it is kept in check by a balance of other bacteria. When the balance is disrupted, usually by taking broad spectrum antibiotics, c. diff can overgrow and release toxins that attack the lining of the intestines, causing a condition called clostridium difficile colitis that is part of an inflammatory reaction, with a “pseudomembrane” formed by a viscous collection of inflammatory cells, fibron, and necrotic cells. The yellow gunk in this image is the pseudomembrane my doctor saw in my colon when my infection was active (yes, that is a picture of my actual colon!).
Side note, my doctor was actually somewhat surprised that my colon didn’t look much more inflamed when he did this colonoscopy. For that I credit my healthy real food “paleo”-inspired diet. Throughout all of this my Crohn’s disease did not flare up and while I did have often severe diarrhea, moderate anemia, and lost weight I couldn’t afford to lose, I was spared the fevers, fatigue, and severe abdominal pain that many with c. diff infections struggle with. For the most part, I was able to continue on with my life as normal – though after dealing with it for more than four months I was starting to get pretty weak and definitely ready to try a new treatment strategy.
Drug resistant clostridium difficile
As I wrote in my last post on the topic, after I was diagnosed in July my doctor prescribed first a 14-day course of vancomycin which seemed to help somewhat but then my symptoms came back shortly after stopping it. This happens in about 20% of patients – likely because the bacteria is spore forming and can lie dormant – so I wasn’t too concerned that I needed a second course. Unfortunately, this time I never had any relief and my doctor switched me to another antibiotic fidaxomicin. At this point my symptoms worsened even more, and it became clear that I was dealing with a drug resistant strain of the bacteria. This is an increasingly common problem, and the Centers for Disease Control has gone so far as to label it an “epidemic.”
The role of probiotics
A lot of people wrote to me on social media and in the comments of my last post that I should try probiotics, which I took throughout the entire time. The specific strain that has been studied and shown to be effective in some cases against c. diff is sachromyces boullardi. I was actually already taking that prior to my diagnosis in an attempt to rebalance the self-diagnosed gut dysbiosis I thought was the cause of my diarrhea and unintended weight loss.
My experience with a fecal microbiota transplant (FMT)
As I wrote in my prior post on the topic, fecal microbiota transplantation (FMT) is the process of transplanting fecal bacteria from a healthy individual into the recipient and it has been shown to be effective for patients suffering from relapsing c. diff infection. Considered experimental for other conditions, it has actually received United States Food and Drug Administration (FDA) approval for use in treating c. diff because of these studies. Because of this, my doctor was able to do the transplant in conjunction with a colonoscopy and bill my insurance (score!).
Step 1: Securing a donor
This is was actually quite easy for me. My husband has the constitution of a horse (that’s a compliment, sweetie!) and was an obvious choice. The best donor is somebody in good health who has not taken any antibiotics for at least 90 days. He was screened for infectious disease through a blood test and a stool sample before being approved.
Step 2: Bowel prep
Again, this wasn’t a very big deal for me because I’ve done numerous bowel preps for colonoscopies and surgeries relating to Crohn’s disease in the past. The purpose of the prep is twofold: to clean out the colon so that the doctor can get good visualization (see my picture above) and to flush out as much of the bacteria as possible. I was on a liquid diet the day prior and then drank the solution as provided in two parts – the night before and then the rest in the morning on the day of the procedure.
Step 3: The donor does his “job”
There are a ton of good jokes that can be made here… Essentially, my husband had to produce a stool that was as fresh as possible, so he tried to time his eating and activity so that he had a bowel movement as close to the time we needed to leave for the hospital as possible. He collected it in one of those “hats” and we brought it with us in the back seat (I admit… that was a little weird. I thought about how we would explain that if we got pulled over…).
Step 4: At the hospital, preparing for colonoscopy
Just like with any other colonoscopy, I was directed to change into a hospital gown and an IV was placed in my arm. At this point, my anxiety level was getting pretty high and I was very grateful for the versed and propofol that soon flowed in! I dozed off just as the nurses started preparing the donor stool off in the other corner of the procedure room.
Step 5: The transplant and recovery
This part I was asleep for, of course. My doctor said he used four syringes of donor stool mixed with saline solution and introduced them into four different parts of my colon so that the whole thing was coated in the new “healthy” bacteria. When I woke up, I was directed to try to avoid a bowel movement for as long as possible and was sent home to recover from the affects of the anesthesia.
The results
Within just a few hours I felt a vague sense of well being that I don’t quite know how to describe. I just felt… good! The next day I had a business meeting and recall driving in my car and thinking the world looked a bit brighter. Perhaps that was all just wishful thinking, but it felt good.
However, my symptoms did not immediately disappear. I continued to have diarrhea and after two weeks a follow up stool test was still positive for toxin A, though I did feel like I was improving ever so slowly. My doctor prescribed another long course of vancomycin, but I resisted taking it. Instead, I asked him to give me some more time and also a prescription for Enteragam – a serum-derived bovine immunoglobulin/protein isolate (SBI) that is generally used for patients with diarrhea-predominant irritable bowel syndrome (IBS-D) or HIV-associated enteropathy to support their nutrition. This was a recommendation from one of my loyal readers – Thank you!
I went on vacation with my family, focused on some serious stress reduction and relaxation while taking the Enteragam and continuing the probiotics. I held onto the vancomycin “just in case” but did not ever take it as my bowel function continued to slowly improve.
Then, last week… almost exactly four months after my initial positive test, I finally got the results I was looking for. All three of the studied samples were negative for c. diff!
The road ahead…
Even though the c. diff toxin is undetectable now, I still have a long road to complete recovery. I need to regain about 20 pounds and I continue to have less-than-optimal digestion and absorption (most of that due to the borderline short bowel syndrome I was left with after my multiple surgeries). The good news is that my Crohn’s disease has not flared up (again, I credit that mostly to diet though I am also taking a prescription biologic).
What I eat now
I call my current diet “paleo-inspired.” I am strictly gluten-free and eat mostly whole and unprocessed foods of the highest quality I can find to continue to promote a healthy gut. That means grass fed meats, organic produce, fermented foods, organ meats, and lots of bone broth. I eat minimal nuts (I don’t seem to digest large quantities very well) and I am on the fence about whether or not I can tolerate dairy. Grass fed butter and cream appear to be fine but I seem to be completely unable to digest lactose now so fluid milk is out. Low-lactose cheese should be fine, but I haven’t experimented it much.
Because I am actively trying to gain weight, I place a lot of emphasis on making sure I get plenty of “safe” starches and carbohydrates in my daily diet. That means that I do eat white rice at least a couple times a week. I also started eating soaked gluten-free oatmeal several mornings a week in an attempt to get more soluble fiber to continue feeding the “good” bacteria my husband generously gave me! This is most definitely NOT PALEO and I definitely struggled with the decision to try it after being mostly grain-free now for almost two years, but it seems to be helping a great deal.
Another challenge I have is that I have difficult digesting large amounts of fat. Not only do I not have a gallbladder anymore, I also do not have the portion of my small intestine that reabsorbs bile acids. The standard advice given to most paleo folks without functioning gallbladders is to take supplemental ox bile so they can eat more fat, but I have to be careful here because it is super easy for me to take too much ox bile, which can cause diarrhea too. It is a constant balancing act but I have found that loading up fat-heavy meals with a corresponding amount of soluble fiber (like that found in oatmeal) really helps.
The lesson here… One size doesn’t fit all. The grain, legume, and dairy-free idea of “Paleo” is a template and one I encourage all people who want to optimize their health to start with, but then be open to customizing to meat your own unique needs.
The future
My health continues to be a work in progress. I like to say that becoming Gutsy By Nature is a journey, and not a destination! I continue to research dietary factors, conduct self experiments, and work closely with my medical care team as I balance the natural healing I’ve found so helpful with the tools that conventional medicine provides.
I sincerely appreciate all the personal messages from you all and hope that by sharing my story here, I am helping someone else struggling with similar issues.
Thank you again for all of your support!
Yours in health,
Jaime


27 replies on “Clostridium Difficile: A Fecal Microbiota Transplant (FMT) Success Story”
I was just diagnosed with c-diff after being sick for 5 weeks but having it for at least 11 weeks. We kinda know when it started due to being on antibiotics while pregnant then getting a lot while I was in labor. I’m on the first round right now. Hope they work since I am so over this and I have a very young baby. My husband only comes home on his days off and during day on weekends due to his job. They did tell me that the transplant is a option but they were trying to avoid it.
I think you have to try the antibiotics to knock out the c diff at least two times before insurance will cover the cost of the transplant. Best of luck to you – hope you are feeling better soon!
Update: had to do two full rounds of treatment and finally kicked it. Side effects: had to stop breastfeeding, lost 20lbs, severe intestinal and esphogus problems. Also caused my body to be seriously vitamin d deficient. Pregnant with #2 and have to avoid all antibiotics, some medications and caused me to be literally sick all through pregnancy. Was on protonix for a long time which helped a lot, but once pregnant they wouldn’t cover it. After 6.5 months they finally covered it again. Back to finally being able to eat. 7 months pregnant and gained 1 lb finally! I work with a dietician to work around food allergies. Had some before, but now most are worse and have new ones. C-diff is no joke and can cause tons of long term problems. I now have precautions I have to follow during birth and for a year after. C-diff is naturally in baby poop for first year. I hope everyone who goes through this knows they are not crazy or alone. It messes you up.
Doctors in the U.S. can actually only perform it for recurrent C-Diff infections at this time. There is no charge specifically for the Fecal Transplant procedure; it is done as a routine Colonoscopy and charged as such.
I had my gall bladder out in November 2020, I received a gift of antibiotics while getting a bladder and kidney infection due to the catheter during surgery, that is when the vicious cycle of CDiff started, 7 months later and 5 rounds of vanco, recieved a fecal transplant yesterday, left with NO answers not sure what to expect. I will take your advice and hope for the best! I have not had a bowel movement since yesterday hopefully the good stuff is working! Should I be taking probiotics? Kefir has been my go to, but my poor gut has been through the ringer! Any how, love all your information!!! And am happy to hear your doing well!
Your story gives me some relief. My boyfriend Jake has been dealing with cdiff and ulcer colitis for over 5 months and it has come back 6 times now. They finally agreed to do the transplant next Thursday. They keep giving him the vancomycin but it hasn’t helped and his side is still hurting no matter how much pain medicine they keep giving him. They tested his mom and she was going to do the transplant, but we found out she has it also just without any symptoms, so we are in the process of testing every family just to make sure no one has it. We have a random donor who will be doing the transplant with Jake. No one in the family has ever heard of this until we had to go through everything. I’m glad to hear/read stories about this because at least I know others have been through it and have had positive results. Hopefully we will get good results from it also.
So an update on Jakes situation: we did the transplant, found out he has celiac disease, and so we went completely all natural, gluten-free, no preservatives, etc. he felt fine for a month and even had some normal bowel movements.. Huge improvement! And the it just went slowly back into his “normal” hurting stage. Bowel movements became diarrhea constantly, I’m talking like at least 12 a day, his side is still hurting in the same spot. They keep switching out meds but his gastro has literally said he has never seen anything like this and doesn’t know what to do. We’ve done steroids, injections, pills, transplant, scopes, flushing him out, and he still has the same symptoms as before. Does anyone know what else we could possibly look for or have a similar story? (crohns was ruled out by 3 drs)
Have they checked him for other parasites? Have you tried seeing a functional medicine doctor? I’m so sorry to hear that he is not doing well. I can’t imagine how frustrating it must be to not have a diagnosis.
Thank you for sharing this story. Unfortunately, fecal transplants are not yet available in Canada, but we’re really interested in their potential to help restore microbiota diversity, as it seems that the absence of specific bacteria may be related to different autoimmune conditions. For example, research suggests that people with autoimmune Psoriatic Arthritis (like my husband) lack Akkermansia & Ruminococcus. Maybe those could be reintroduced through a fecal microbiotia transplant?! If so, we’d have to travel to the States or somewhere else where fecal microbiotia transplants are available. (That research is available here: http://onlinelibrary.wiley.com/doi/10.1002/art.38892/epdf).
[…] Hartman is the blogger behind Gutsy By Nature. She has Crohn’s disease and received a fecal microbiota transplant last year for a recurring C. difficile infection. Her husband was the donor, and her gastroenterologist in […]
[…] UPDATE (November 23, 2014): Success! Read my follow up post here. […]
[…] Hartman shares a 1st-person account of a successful fecal microbiota transplant on her blog Gutsy By […]
[…] I’m so grateful to friend and fellow IBD/food blogger Jaime of Gutsy by Nature who bravely battled C. diff recently and who kindly became my sounding board for what to expect after an […]
[…] my colon is in good shape and my Crohn’s disease seems to be under control and beating the nasty c diff infection that I struggled with all summer and into the fall. It feels like I’m constantly taking a […]
I found your website through pinterest and I’m super grateful! I was diagnosed with c-diff the first time on 9/1 after a few days in the hospital for Mono. I take a 5-ASA for colitis, which was in somewhat of remission earlier in the summer. I took vancomycin for 14 days, and thought I was doing better. But after another week of trouble, I called my doctor. Yesterday’s test came back positive, and he just prescribed dificid, which is super expensive. It was good to read about the transplant you had as someone just suggested that to me. Thank you for sharing what did and did not work for you, and also that there is a form of c-diff resistant to medication.
I’m so sorry that you are suffering with c diff as well. I hope the difficid works for you but if not, the transplant has an amazing success rate! Please keep me posted as to how you are doing. Will be thinking of you!
Thank you for this post. I’m not exactly sure how I stumbled upon it but it gave me some encouragement that even with failing treatments this is so helpful. I’m 5 months in to my first Crohns flare in 6 years. I contracted C diff on top of tha after my first hospital stay. I can’t even count how many rounds of antibiotics and constant steroids I’ve been on with still no relief. We’re in a tight spot not wanting to do a colonoscopy because my inflammation is so out of control. Hoping this stand still ends soon and I can make some progress. I’m @dallassrae on Instagram if you want to connect. Thank you
Thank you for writing Dallas. I’m so sorry that you are dealing with this too and hope that you start to feel better soon. Have you talked with your doctor about a FMT?
I am so thankful to have stumbled upon your blog post. I was diagnosed with c diff in December after being put on two antibiotics in November after wisdom tooth surgery that had complications. In December my symptoms were so severe as well as the pain and I lost so much weight I was hospitalized for two weeks in isolation. I was tried on both oral and IV flagyl but both failed so ended up on vancomycin for 14 days. Well I just finished the vancomycin one week ago and now as of yesterday the c diff is back. I had diarrhea with severe bleeding so I wound up in the emergency room. I had a bunch of bloodwork and tests done and have now been prescribed a MONTH of vancomycin. I am so nauseous and my stomach is in agony. A gastroenterologist is going to follow up and scope me in the next couple of weeks.
Thanks for bringing awareness to this awful disease that does not just affect our elderly or immunocompromised.
I hope you are feeling better soon! Hoping the longer course of vancomycin does the trick for you… please keep me posted.
After having severe diarrhea for 5 weeks (after being on antibiotics for an infected tooth), my doctor diagnosed me with C Diff and put me on 2 weeks worth of antibiotics (can’t remember what kind). After completion of the antibiotics, my stool was still very loose, however, I no longer had pain. The test came back positive for C Diff once again, so the doctor put me on a round of different, stronger antibiotics (again, not sure what it was called). I just completed this second round of antibiotics and still have loose stool. I’ve been wanting to follow a more paleo-friendly diet, and have been keeping at least one of my daily meals gluten-free, but obviously, that isn’t enough. Your story has given me that extra push I needed to go completely (almost) gluten free! I hope this works! Keep your fingers crossed!
At the very least, having a good diet will help you keep up your strength as you battle the c diff. I hope this round of antibiotics works!
Excellent post and very helpful. I was just diagnosed two days ago. I got it from a strong antibiotic treatment to kill H Pylori (another nightmare).
I feel hopeless. I am glad to read your post and it’s helps give me a glimmer of hope back.
I have read that going meatless is very bebeficual. I notice you include meat. Doesn’t thus bother your stomach??
I do not believe that going meatless is beneficial. Obviously there are others who disagree, but I am convinced by personal experience and the science that humans are omnivores and that consuming protein and fat from healthy animals is crucial for optimal health.
Hi there… I know this is an Old post, but I was curious how after only 4 months your Dr suggested an FMT? I was diagnosed 7 months ago with my 1st bout with a severe bacterial infection by the ER and CTScan but I have yet to have any Dr even discuss the FMT, I only know about it from doing my own research.
I have lost over 40 lbs since all this started and I am now on my 4th round of Antibiotics. My stomach is a wreck and its difficult to even eat.
I am not sure where to turn. I have another apt with the Gastro in a few weeks but in the meantime, might you have any suggestions for me? Im doing probiotics 2 hours after each dose of antibiotics (Flagyl every 8hr and Ciprofloxacin evry 12 hr). My Ins will not cover Vancomycin.
I would appreciate any feedback you can offer.
Sincerely,
Tiara
You may need to bring it up first and push your doctor, either to do it him/herself or to refer you out to someone who will do it. FMT is an approved and validated treatment for clostridium difficile and so any gastroenterologist should at least be able to speak about it.
Ask to have vancomycin compounded it is so much a better price.